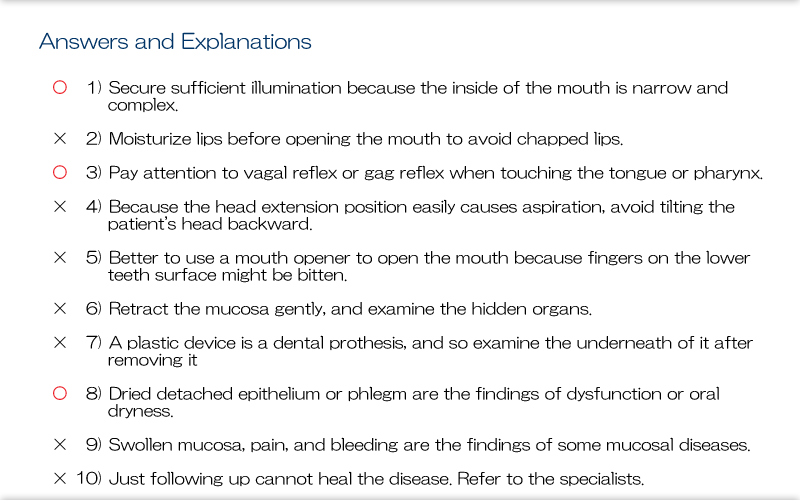
Explanation
The oral cavity comprises soft tissue such as mucous membranes and hard tissue, and it is morphologically and functionally complex. As a narrow space not easily penetrable by light, the darkened cavity is difficult to examine in detail. So, to examine for oral disease and disorders and provide oral care, we need to illuminate the cavity.
This module explains techniques for examining the oral cavity and some considerations.
Explanation
This slides show the main topics covered in this module: ① methods for examining the face and oral cavity, ② the normal appearance of the face and oral cavity, ③ dental prostheses for the oral cavity, and ④ abnormalities on the facial surfaces of the teeth and in the oral cavity.
Explanation
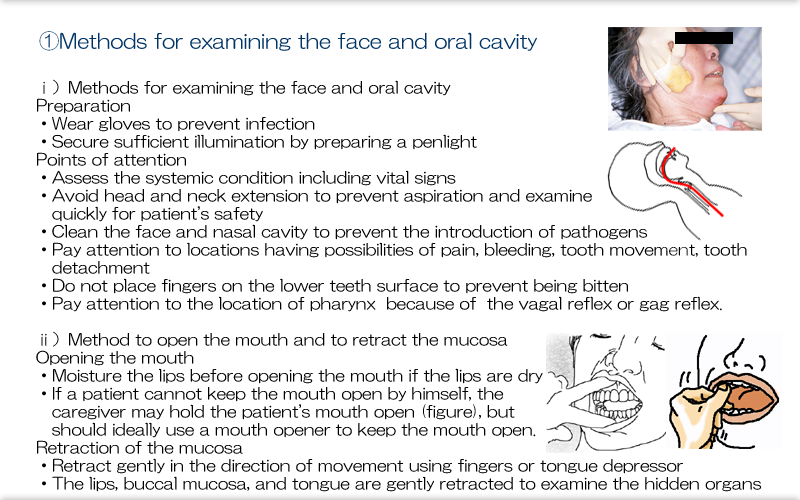
Observatory procedure will be described. Wear gloves to prevent infection and secures sufficient illumination. The examination begins with determining both the systemic and local status following a checklist of items that must include vital signs, paralysis and contracture, aspiration risk, feeding status, maintenance and duration of suitable posture and any effect of posture on vital signs, dentition and dentures, and tools used for oral hygiene.
Avoid head and neck extension to prevent aspiration and examine quickly for patient's safety.
Touch the oral cavity after cleaning the face and nasal cavity to prevent the introduction of pathogens, . Pay attention to the fall of moving teeth or dental prostheses to prevent aspiration. Any painful soft tissue should be retracted gently. Uses fingers to open the mouth and may use a device to keep the mouth open. Any time a speculum is used in the oral cavity, careful attention is needed to avoid losing any loose teeth and injuring the mucous membranes. Careful handling is needed when touching the pharynx or base of the tongue because it may cause the vagal reflex or gag reflex in.
Moisture the lips when opening the mouth. If a patient can not keep the mouth open by oneself, the examiner may use his or her fingers to hold the patient's mouth open, and use a mouth opener to keep the mouth open.
The lips, buccal mucosa, and tongue are gently retracted with a tongue suppressor or his or her fingers.

Explanation
Before touching the oral cavity, the examiner should check the patient's face for any findings suspicious of systemic disorders. The patient is examined for facial morphology, symmetry, complexion, pain, muscle function, and nasal breathing hygiene. Also, the lips are examined for color, dehydration, hygiene, and functional performance.
Explanation
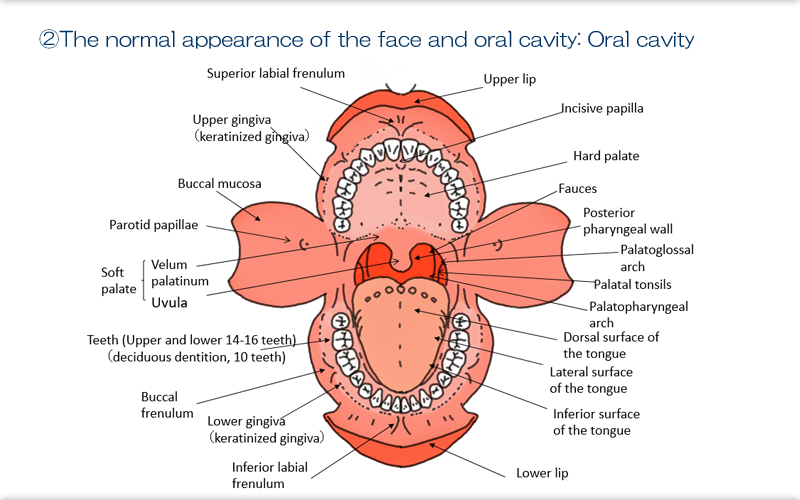
The oral cavity is enclosed by the lips, the posterior pharyngeal wall and palate superiorly, the floor of the mouth inferiorly, and the buccal mucosa laterally, and it functions as the entrance to both the alimentary canal and the respiratory tract.
Adult dentition comprises up to 32 teeth in total (including wisdom teeth) in the mandibular and maxillary arcades. In infants, deciduous dentition consists of 20 teeth, and both permanent and deciduous dentition may be present during the period when permanent teeth are erupting and replacing deciduous teeth. The membranes surrounding the teeth are called the keratinized gingiva. The gingiva are immovable membranes, so they are distinguished from the moveable mucous membranes, the buccal, sublingual, and pharyngeal membranes. Where teeth have been lost, they may be replaced by dentures on the gingiva.
The tongue is muscle. Its dorsal (upper) surface is rough due to the presence of keratinized lingual papillae, and its ventral (lower) surface is characterized by a pale soft membrane.
Explanation
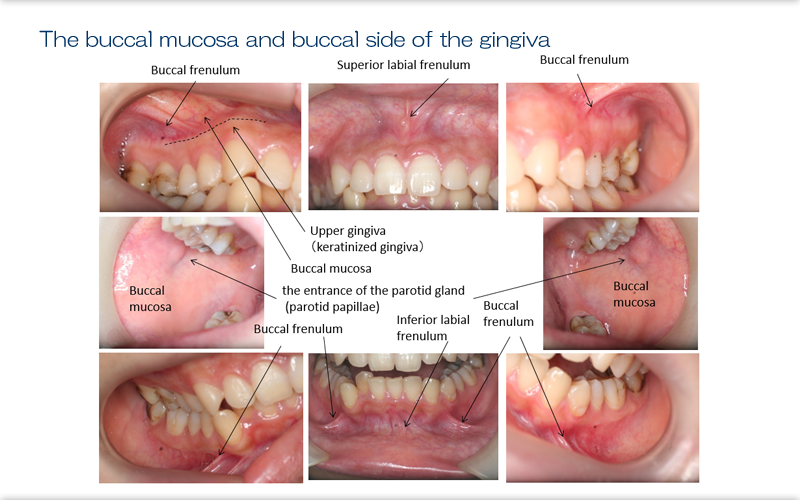
When the patient's mouth is open, the buccal mucosa and buccal side of the gingiva can be observed with retraction of the lips and buccal mucosa. The top photographs here show the lips and buccal surfaces in the maxillary region. In the regions of the left and right upper molars, the periodontal gingivae are connected to the buccal mucosa, and retraction of the buccal mucosa reveals the muscle-like superior labial frenulum (top middle photograph). The superior labial frenulum is directly continuous with the center of the upper lips. The frenulum and surrounding area is prone to ulceration from dentures, and it is also prone to accumulation of food residue with functional deficits or paralysis.
The left and right middle photographs show the buccal mucosa at the point the mouth is opened. Arrows indicate the openings of the saliva-producing parotid gland (the parotid papillae). Decreases in parotid-gland salivary secretion due to factors such as age, dehydration, and adverse drug reactions are common. When examining the oral cavity, the region corresponding to the parotid gland in the cheeks anterior to the ears should be retracted to check the flow (both amount and quality) of saliva from the parotid gland.
The bottom photographs show the buccal surface over the lower jaw. The gingiva, buccal mucosa, buccal frenulum, and the inferior labial frenulum (connected to the lower lips) can be examined.

Explanation
When the mouth is open, the palate, pharynx, tongue (dorsal and sublingual surfaces), and teeth (occlusal surfaces and palatal and lingual aspects) can be examined.
The upper left photograph shows the palatal side of the maxillary dentition and the palate. In patients with oral dryness (xerostomia), there may be a buildup of detached epithelial cells, saliva, and bacteria in many places, and thus check the palate carefully with the light.
The middle left photograph shows the palate with the movable tissue of the soft palate posterior to the hard palate (velum palatinum, with the uvula in its middle). The region running to the left and right sides is the palatoglossal arch. Posterior to this arch, there is the palatal tonsils, with the palatopharyngeal arch, and the posterior pharyngeal wall is at the back. In some pediatric cases, the tonsils are clearly enlarged, leading to the problem of mouth breathing.
The lower left photograph shows the dorsum of the tongue. A coating on the tongue is often seen in patients with oral dryness or impaired tongue function; it is important to check for any coating adhering to the tongue and its characteristics. A healthy dorsum is moist and slightly rough to the touch due to the lingual papillae. However, systemic conditions such as anemia and immunosuppression make the tongue smoother. Other manifestations in such conditions include extension and discoloration of mottled papillae and a dry, adhesive buildup, leaving the patient prone to systemic effects.
The upper right photograph shows the area of below the tongue with the mouth open and the tongue inverted, and the lower right photograph shows the floor of the mouth. The band running sublingually along the midline of the floor of the mouth is the lingual frenulum. The region traversed by submandibular ducts and with the opening of the sublingual gland is called the submandibular fold, and the submandibular duct opens into the sublingual caruncles. Facing these structures, we have the lingual aspects of the front teeth in the mandibular arcade, to which tartar (calculus) can easily adhere.
Explanation
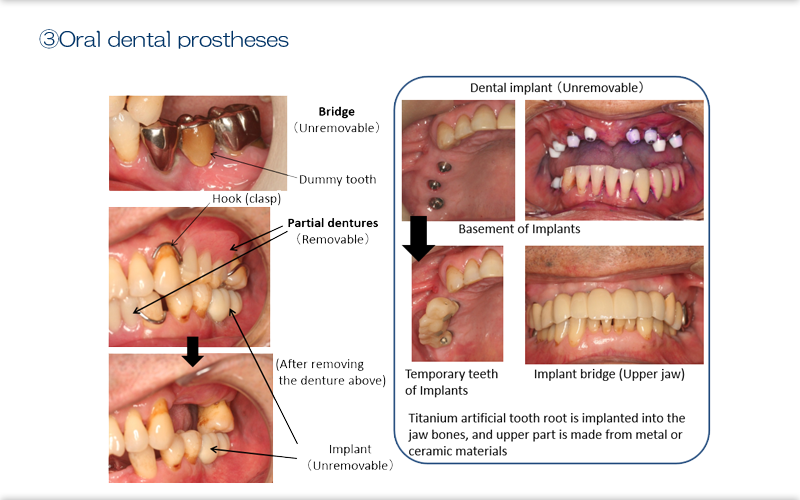
1) Oral dental prostheses
Oral dental prostheses are artificial and are made with metal, plastic, or ceramic materials.
The underside of an oral dental prosthesis borders on the gingiva, and gingivitis readily occurs with the buildup of food debris or other matter in this border region. Remove removable dentures (complete or partial dentures) and them cleaned them outside of the mouth and checked if there is gingival inflammation underneath the denture.
2) Tissue changes associated with dental prostheses and dental prosthesis abnormalities
When patients have 'dummy teeth' with bridges or bridge implants (teeth that are ostensibly not connected to the root), a gap is artificially created between the underside of the dummy tooth and the membrane. Piled up plaque under the base of a dummy cannot be easily removed with cleaning, so checks the area carefully even when this area seems clean at first glance.
A wobbly dental prosthesis can indicate that the prosthesis itself is coming loose, but it could also represent a prosthesis becoming detached from the tooth; careful attention is needed to avoid detachment and subsequent accidental ingestion or aspiration during cleaning. Partial dentures are held in places with hooks or clasps, which are thin metal objects that can easily lead to misshapen dentures when attached incorrectly. A misshapen dental prosthesis becomes a poor fit, and as it further loses shape, the hook can puncture the membranes. So, verify that there is no loss of shape at the time of attachment.
Explanation
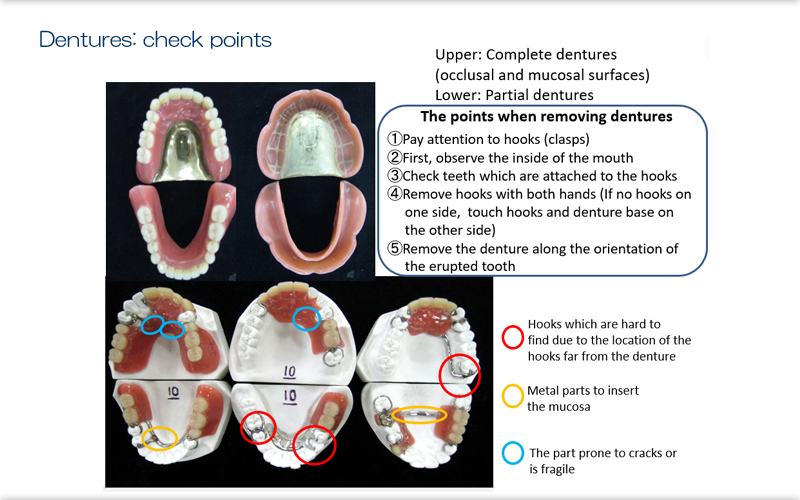
3) Understanding maintenance of removable dental prostheses
Check if removable dental prostheses (complete or partial dentures) works properly. The status of their use (eg, independent cleaning, attachment, and time of use) should also be checked.
Check in the oral cavity include looking for any loss of teeth to which hooks are attached, whether hooks have become misshapen, if dentures are cutting into the membranes, and gingivitis. These findings suggest poor fitting of dental prostheses.
Check outside the oral cavity include establishing that the hooks are not misshapen or damaged, that there are no artificial teeth missing, and there are no cracks or sharp edges in the denture floor (pink plastic portion) or fractures of the artificial teeth.
These are the points for attention when removing dental prostheses. First, while checking for places where the hooks are attached inside the oral cavity, use the fingers of both hands to grasp the dentures on the left and right sides (unless the prosthesis has been installed unilaterally). Then, remove the prosthesis along the orientation of the erupted tooth, and remove it from the mouth. Gloves must be worn to prevent any injury from hooks or sharp teeth.

Explanation
The next step is to assess dentures. The contaminants adhering to the denture can be "hard" or "soft". Hard contaminants refers to tartar (hardening of calcium and phosphorus calculus). Soft contaminants refers to plaque that have developed with prolonged retention of fungal or bacterial biofilm and food debris. Dental calculus cannot be removed by brushing the artificial teeth, so it must be removed at a dental clinic. Biofilm, plaque, and food debris can be physically cleaned off by brushing with a toothbrush for artificial teeth. Dental plaque is the cause of decay of the remaining teeth, inflammation and swelling of the gums, ill-fitting dentures, damage to the gums (denture ulcers), and inflammation of the membrane under the dentures. It has also been reported that bacteria adhering to dentures cause aspiration pneumonia. In many cases, elderly or disabled patients are unable to manage their dentures by themselves, so the state of denture hygiene and handling can be the information about the patient's surrounding environment.
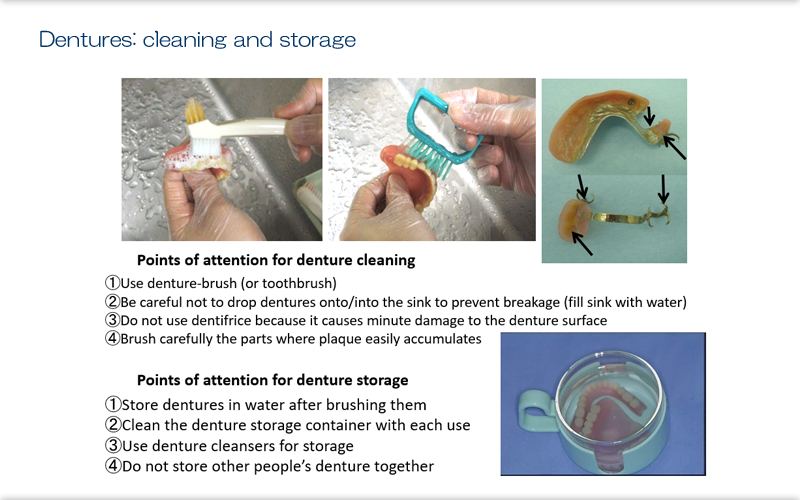
Explanation
Denture plaque can cause dental caries on the remaining teeth (decay), inflammation of the mucous membranes on the gums, and denture ulcers, as well as aspiration pneumonia. It is essential that chemical cleaning (with denture cleansers and antiseptic solutions) is preceded by physical cleaning using a specialized toothbrush for dentures because chemical cleaning alone does not have a sterilizing effect against the deepest bacteria in the biofilm that develops on dentures. Dentures are made to fit the shape of the patient's oral cavity, so their shape can be complex, and it is important to be aware where buildup might occur and apply brushing there. Dentifrice such as toothpaste must not be used when brushing dentures because it causes minute damage to the denture surface, making them prone to microbial proliferation. After removing dentures before sleeping, the removed dentures should be soaked in water (although there are cases where the patient may sleep with dentures fitted; the dentist's instructions should be followed). Dentures become misshapen, cracked, or damaged when they dry out, because they contain water-absorbing resin material. However, when unclean dentures are placed in water, microbes proliferate in that water, and an adhesive biofilm develops in the container.Thus, both dentures and the container must be cleaned before placing the dentures in water overnight.
Explanation
Abnormalities of the oral cavity
Hygiene
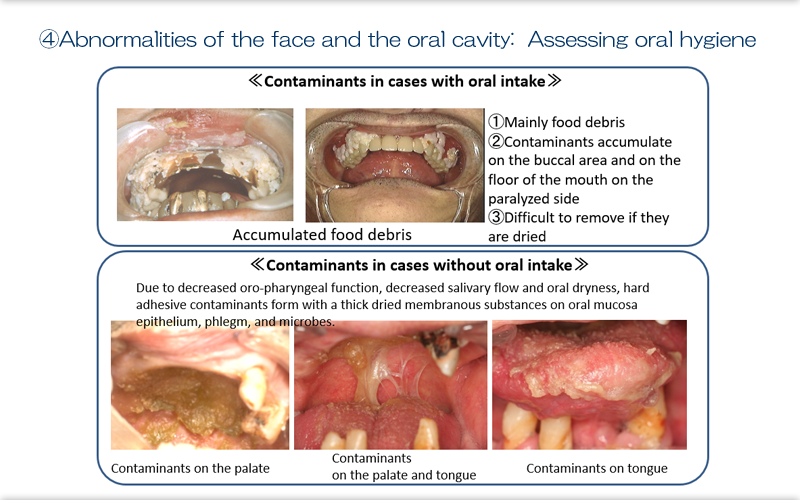
i) Food debris in the case with oral intake
When oral hygiene is not satisfactory in patients who eats orally, food debris leads to the growth of bacteria, and the resultant plaque is the main source of contaminants on the teeth. With intense dryness, the contaminants dries out and becomes harder, which is then more difficult to remove. When patients have facial paralysis, contaminants occurs on the buccal area on the affected side and on the floor of the mouth.
ii) Dried detached epithelium and contaminants in the case without oral intake
When patients don't eat orally, salivary flow decreases, oral dryness intensifies, and a hard adhesive contaminants form with a thick detached epithelium, phlegm, and microbes. This adhesion may occur on the lips, teeth, palate, tongue, and pharynx, and large quantities of residue may accumulate in the pharynx with loss of pharyngeal function.
This hard contaminants is difficult to discern unless the area behind the upper front teeth and the anterior palate are illuminated. It is important to identify any hard buildup though, because it is suggestive of functional deficits such as impaired tongue functional or reduced salivary secretion.

Explanation
iii) Periodontal disease and caries because of long-term inadequate dental hygiene
Periodontal disease and dental caries occur when oral hygiene is persistently poor and salivary secretion is reduced (as an age-related change, dehydration, drug effect, or other change). With progression of periodontal disease and swelling of the gums, brushing causes pain and bleeding in the gums, and oral hygiene deteriorates further. Over time, the roots of the teeth become visible, and this often leads to decay at the root surface (cervical caries). Progression of decay of the root leads to ill-fitting dentures and further difficulty with dental cleaning. If a tooth breaks at the root, patients are left with a stump (attention is also needed to prevent loss, ingestion, and aspiration of the tooth at the time it breaks). When root surfaces are exposed, these teeth lose bone support and become loose. This causes pain and difficulties in removing buildup from teeth that wobble during brushing, and there is also a risk of tooth loss, ingestion, or aspiration during cleaning. Loose teeth that appear to wobble up and down may require extraction, grinding, or fixation because there is a high risk of loss. With ill-fitting dental prostheses and tooth decay, misshapen teeth become more difficult to clean, and this creates a vicious cycle of progressive periodontal disease.

Explanation
Findings suggestive of functional impairment
Oral manifestations of systemic disorder
The mucous membranes of the oral cavity continue to the alimentary canal and represent tissue with an active role in metabolism, which explains why they can show symptoms of system disorders. A smooth tongue and painful stinging in the tongue (glossitis) can occur due to anemia and malnutrition. Candidiasis and herpes virus infections are frequently seen with immunosuppression. Denture ulcers brought on by ill-fitted and unsatisfactorily cleaned dentures and denture candidiasis are not systemic symptoms and these findings are related to the condition of the dentures.
Abnormalities related to dysfunction
We frequently see an increase in tongue coating due to impaired tongue function and oral dryness due to salivary secretion. A black hairy tongue indicates more than just impaired tongue function; it is related to the normal oral microbiota being replaced by microbes with long-term antibiotic treatment, and decreased salivary secretion is related to systemic factors such as adverse drug reactions, stress, and dehydration.
Oral mucosal diseases Oral mucosal diseases that can be observed on the buccal mucosa, tongue, and floor of the mouth. The mucosal diseases include stomatitis, aphtha (small mucosal ulcers that are painful to touch and associated with a sour taste), and pemphigus, an autoimmune disease involving the entire mucosal surface (membrane detachment and evident pain).
Explanation
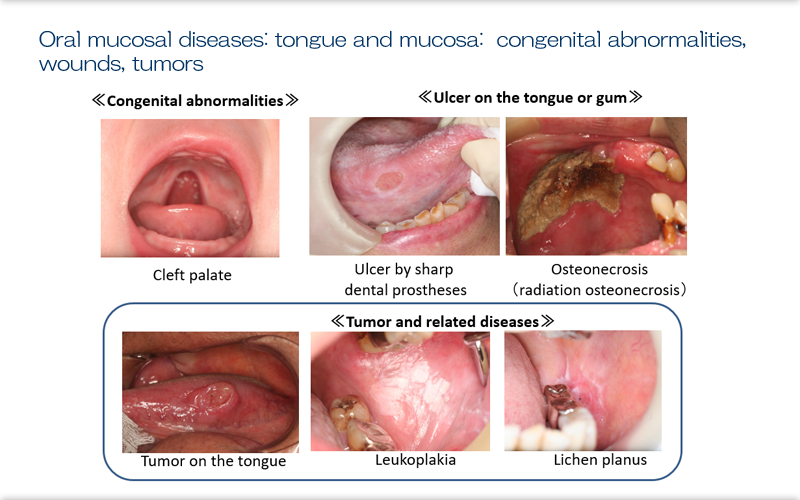
Here we can see a range of congenital abnormalities, including cleft palate where the palate is cleaved (or cleft lip and palate when the cleavage extends to the lip), ankyloglossia, and fissured tongue. For disabled children and others with respiratory disablement, we may also see congenital absence of the jawbone, a functionally constricted dental arch, and/or a high-arched palate; however, the relevant details are described in the other module.
The membranes of the oral cavity are uniformly thin and, unlike the skin, lack a cornified layer (although the gingiva is keratinized, it is very thin). So, damage to these membranes can easily occur from a range of causes. Ulcers can form because of sharp teeth or dental prostheses and accumulation of food debris under dentures. These ulcers are painful and result in the patient eating less as well as establishing routes for microbial infection. These abnormal findings and the disorders that can cause them need to be detected and treated early. The jawbone lies directly below the thin membranes of the oral cavity, and microbial infection frequently follows tooth decay, periodontal disease, and membrane damage, with inflammation spreading to the bone. Immune function, blood flow, and metabolism can be decreased with systemic diseases or drug effects, and cures are likely to be partial, with the patient's condition developing to osteomyelitis or osteonecrosis.
Tumorous lesions are suspected when elevations in uneven membranes and ulcers are seen. Tumors can progress without showing any symptoms and may be discovered as a reason for ill-fitting dentures. We are not just concerned with cancers of the oral cavity; we must also pay attention to leukoplakia as a precancerous lesion (white patches that cannot be removed) or lichen planus (lace or mesh-like white spots on the membranes), which may undergo neoplastic transformation. If these membranous diseases do not resolve on follow-up, referrals for specialist examination and investigation should be made at an early stage.
Recommended readings
- Kikutani K. (ed.): Learning Oral Care from the Basics (in Japanese), 2nd edition. Gakken
- Watanabe Y. (ed.): Resolving Issues in Oral Care (in Japanese), 1st edition. Gakken.